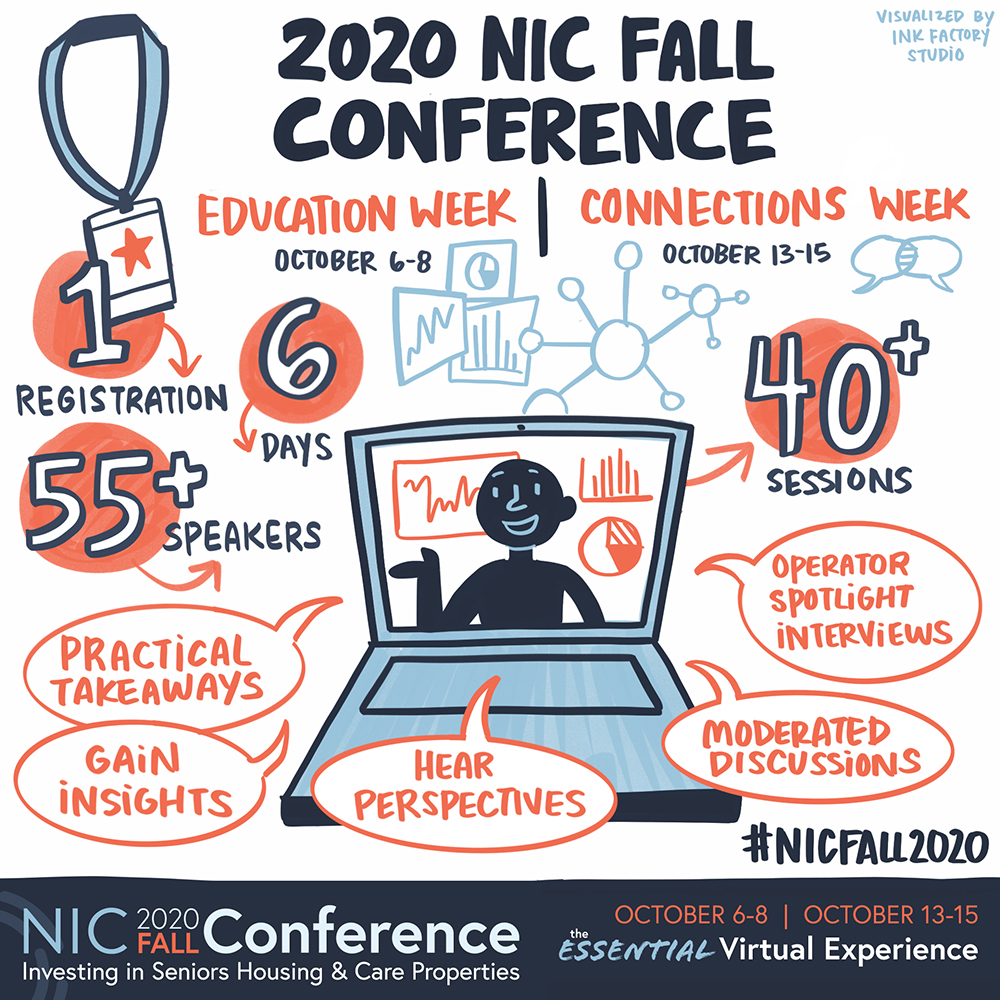
The seniors housing and care sector’s most important annual event will be virtual – but don’t make the mistake of thinking it’s become just another webinar. While the 2020 NIC Fall Conference does share a few features with other events that many of us have attended in this year of virtual conferences, it stands apart as a truly interactive, socially engaging convening of leaders, full of opportunities both to share knowledge and to connect with peers.
In short, the ‘essential virtual experience’ is unique, powerful, and well worth your time. Here are just some of the features and experiences you can expect to encounter, as you and your team prepare to gain maximum value from the many opportunities offered at ‘the NIC’ this year. In many cases, the event incorporates virtual technologies that simulate in-person experiences while others are unique to an online environment.
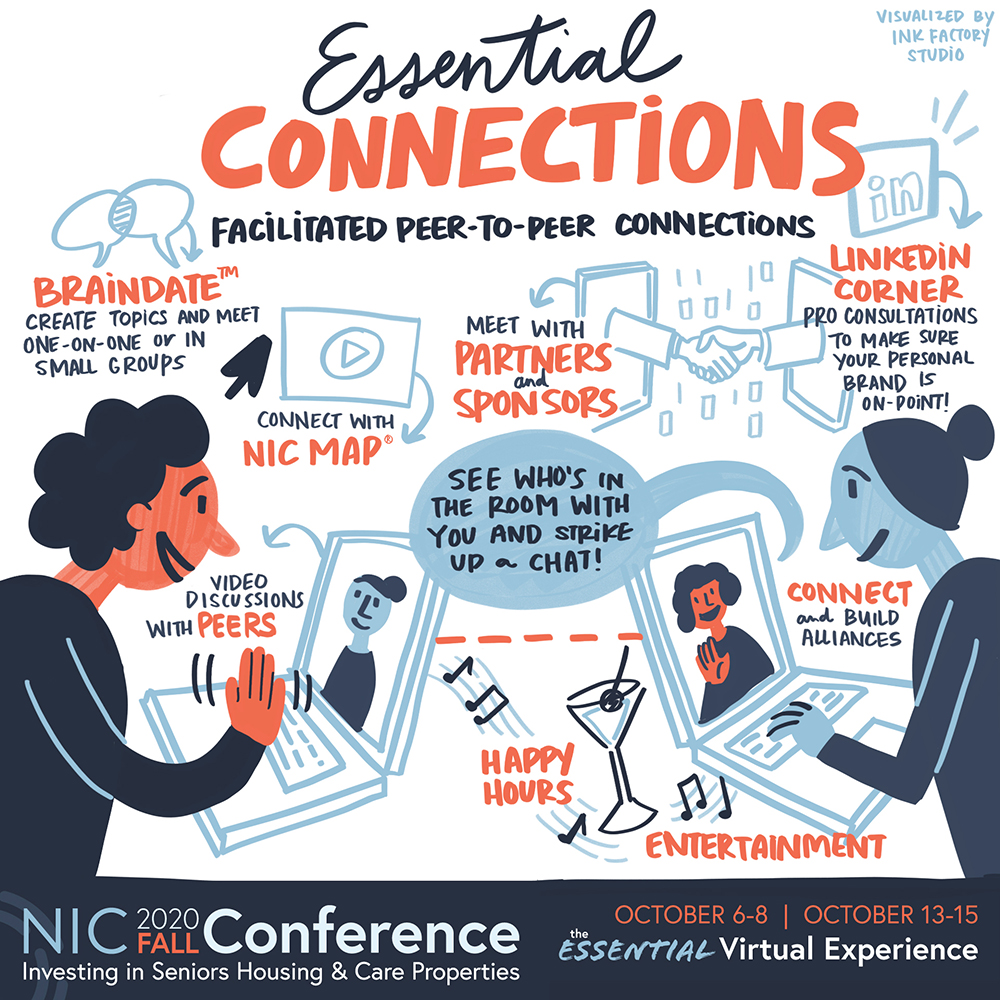
Bump into Friends and Say Hello via Video Chat
The “Essential Virtual Experience” event platform will enable you to see who’s in the room with you, allowing for the kind of chance encounters many attendees experience as they move through a traditional conference. See someone you know? Send a chat to say “hello.” Better yet, invite someone for a video chat to talk one-on-one for up to 10 minutes. You may run into attendees in the virtual Lobby, in the Connections Lounge, or in the Partner Spotlight Zone. You will also be able to see who else is viewing an educational session. Throughout the conference, you can also send and receive emails inside of the event platform, so be sure to check your inbox often.
Peer-to-Peer Connections
Join your peers to share perspectives on timely industry topics. The discussions within the Peer-to-Peer Connections are geared towards creating a community of dialogue on emergent ideas that can provide fresh perspectives and innovative approaches. Gaining insight on how fellow industry professionals are tackling hot button issues can make all the difference in how you navigate your business as you explore various options and potential paths forward. This forum is open to all interested participants.
The NIC Community Connector™
Perhaps the most exciting innovation tied to this conference is the launch of the NIC Community Connector. All attendees who complete the profile registration gain exclusive, complimentary access to NIC’s powerful new networking platform; a custom designed ‘LinkedIn’ style system built to suit the needs of capital providers, owners, operators, service providers, and other stakeholders across the seniors housing and care sector. The innovative online platform provides a means to search for potential new contacts, and to communicate directly with decision-makers.
While launching in parallel with the 2020 NIC Fall Conference, the complimentary NIC Community Connector will remain accessible to all attendees through the end of the 2020 calendar year. Subscribers will retain their access to a powerful set of tools that will streamline efforts to identify financing partners, seek property transactions, and build and grow networks.
The NIC Community Connector is now live. With a completed profile registration, you can now connect with others and access the Attendee Listing. Also, keep checking the platform, as more people sign up, the more powerful it will become. Look for new features, which NIC will continue to rollout this year, providing subscribers with ever-more sophisticated year-round networking capabilities.
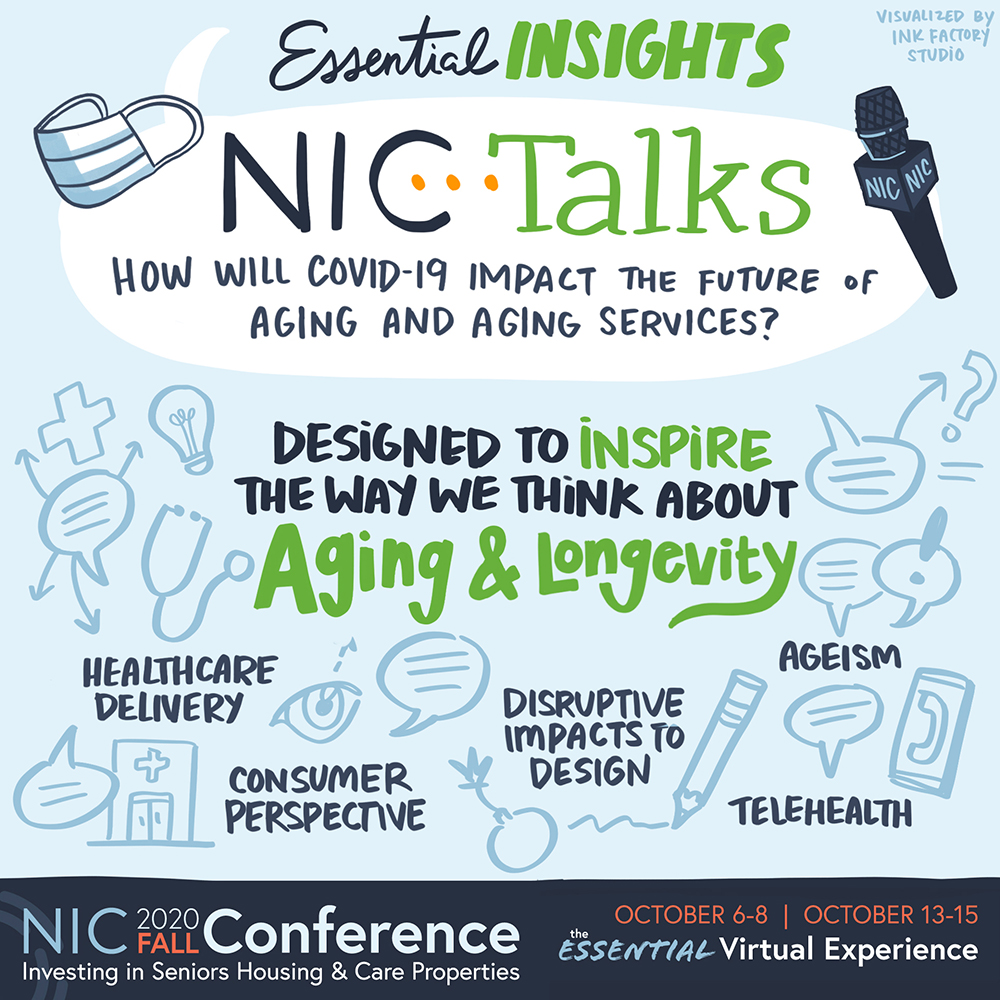
Don’t Miss NIC Talks
Our popular NIC Talks series returns—featuring another group of uniquely qualified, passionate thought-leaders, including business leaders, academicians, and leading advocates, sharing their perspectives on the question, “How will COVID-19 impact the future of aging and aging services?”
Presented in the style of “TED Talks,” these popular sessions often pack a powerful punch. Attendees can look forward to viewing the presentations (available on-demand for convenience) in the first ‘Education’ Week of the conference. During the second ‘Connections’ Week, attendees can participate in Zoom calls, led by some of the NIC Talks presenters, for interactive group discussions.

Schedule Your One-on-One LinkedIn Consultations
Veteran attendees know that NIC conferences often feature a ‘LinkedIn™ Corner,’ complete with LinkedIn experts, to help them take their online networking platform to the next level. This year is no different. Book appointments with branding experts to receive one-on-one 30-minute live video coaching sessions to discuss how to maximize your LinkedIn profile to build your brand. Appointments can be scheduled now and will take place daily during Connections Week (October 13-15) from 1:00–5:00 p.m. EDT. There are only 48 slots available, so book early!
Virtual Rooms
The virtual environment mimics our typical in-person conference space. Just as you might familiarize yourself with the conference physical layout, we recommend you survey the landscape of our online event. Don’t worry, the space is intuitive and easy to navigate, well-signposted, and can be fully traversed with the click of your finger.
Lobby
The Lobby is your home base. It is the central hub from which you can access most of the rooms of the virtual event platform. Don’t forget to look around you and see if any acquaintances are there with you. In this environment, just as in person, you can wave and start a conversation.
Partner Spotlight Zone
Visit NIC’s Premier and Official Partners to connect with their company representatives in the Partner Spotlight Zone. Be sure to make those essential business connections. From here, you can also watch the short videos of Partner Highlights, well worth viewing, particularly if you’re engaged or considering engaging with them in your business.
Connections Lounge
An all-purpose networking space, the Connections Lounge is the place to go for a host of opportunities to see and be seen, and engage with peers during both weeks. This room hosts public chat sessions, video happy hours, one-on-one LinkedIn consultation scheduling (reserve an appointment early), and provides access to the NIC Community Connector and the braindate™ platform.
Main Stage
NIC will host our keynote sessions as well as a few entertainment offerings on the Main Stage. Don’t miss award-winning journalist Soledad O’Brien, moderating a discussion with Mark Parkinson, president and CEO, American Health Care Association (AHCA) and National Center for Assisted Living (NCAL), and Andy Slavitt, senior advisor for The Bipartisan Policy Center and former Acting Administrator of the Centers for Medicare and Medicaid Services. Here, household names and political commentators David Brooks and David Gergen will turn their considerable expertise and experience – and wit – to shed light on the factors to consider as November 3 approaches. This election has the potential to impact the seniors housing and care sector both directly and indirectly, and many attendees will be watching this discussion closely.
Concurrent Sessions
You will come to this room for educational sessions, peer-to-peer video connection sessions, wellness sessions, and NIC MAP® Data Service user group peer-to-peer discussions. You can also come here to see what sessions are coming up, and which ones are currently taking place. Most sessions are available on-demand once they have taken place. Simply visit this space and find the sessions you wish to review at your convenience. Session details and schedules are here.
NIC Resource Center
In the NIC Resources room, attendees can access NIC publications such as the just released NIC Investment Guide, Sixth Edition, and the Seniors Housing & Care Journal 2020. Links are also provided to access, and subscribe to, the NIC COVID-19 Resource Center, NIC Notes blog, and NIC Insider newsletter.
NIC MAP® Data Service
Come learn about the sector’s premier provider of seniors housing and care data, NIC MAP Data Service, in this room. Attendees may schedule a NIC MAP Data Service demo, or simply chat with a NIC MAP representative about their needs and how the data service can help their business. Information will also be available for download.
Executive Insights
NIC has created important benchmarks on the impact of the COVID-19 pandemic on seniors housing and care that will allow the market to be better informed on a timely basis. Surveys are distributed on a biweekly basis. From the Lobby, attendees can access Executive Survey Insights – Market Fundamentals data and analysis on the impact of COVID-19 on occupancy rates, move-in and move-out rates, development pipelines, staffing, and supports for frontline community employees and staff.
Operators can also come here to participate in the survey – an important means to improve transparency, which builds trust, as well as to contribute to greater understanding of the impact of this pandemic on the industry.
NIC Actual Rates
The NIC Actual Rates Initiative is driven by the need to increase transparency in the seniors housing sector and achieve greater parity to data that is available in other real estate property types. The reporting by the NIC MAP Data Service of accurate data on the monthly rates that seniors housing residents are actually paying compared to properties’ asking rates helps the sector achieve this goal.
Enter this space to schedule a meeting or chat directly with a NIC Actual Rates representative to learn more about this important NIC initiative, or to download more information.
Take a Moment for Yourself
In keeping with traditional NIC events, the virtual experience offers opportunities for personal enrichment and relaxation. Take a break to focus on yourself and join in the fun for a special shared experience. There are so many opportunities to interact with peers, thought-leaders, and prospects, that it’s important to take these breaks before heading back into the fray.
Brand, Brain, and Being Sessions
This series of sessions offers attendees a chance to focus on themselves and gain expert insights on improving personal brand, productivity, creativity, and overall wellness. The ‘Brand’ session offers advice on improving your personal brand to showcase your best self. In the ‘Brain’ session, attendees will learn how to build life-changing habits and explore some of the apps and tools they can use to boost productivity, time management, creativity, and new ways to create value. The ‘Being’ session focuses on mental and physical health, featuring tips on wellbeing, advice on essential oils, how to avoid burnout, how to be happy, and self-love.
Hamilton and Young@Heart Chorus


The NIC always exceeds expectations, not only for pure business value, but among the best perks of the year. This year, allow us to transport you from live networking and industry thought-leadership (for an hour or so) with exclusive performances from Broadway’s most popular show, as well as one of the most unique, engaging, and inspiring groups performing today.
Hamilton
Go behind-the-scenes with stories from the already legendary show, and be transported, as Broadway and film cast members perform exclusive “Hamilton” songs that are simply not to be missed.
Spend some time with the Grammy Award-winning New York vocalist, Sydney James Harcourt, who played Aaron Burr on Broadway, featured in the Disney+ film, and also performed in the famous Obama White House performance.
Lexi Lawson made her Broadway debut replacing original cast member Phillipa Soo as Eliza Hamilton in 2016. Fans also know her from the leading role in the first national tour of “In the Heights,” as well as her portrayal of Mimi in the “Rent” national tour.
Young@Heart Chorus
Ranging in age from 77 to 92 years old, the Young@Heart performers prove you can grow old without growing boring. With over 50 international tours under their belts, their musical careers were launched long after retirement.
Don’t worry. Like many sessions, these special entertainment break sessions will be available on demand, to fit your busy schedule.
For further details on all the above, as well as schedule information, and other Conference-related resources, please visit the NIC 2020 Fall Conference event site.