Updated November 23, 2021 (original blog posted June 29, 2021).
The primary tool CMS has for enforcing care standards at skilled nursing properties are civil monetary penalties (CMPs), which are essentially fines for facilities found to be out of compliance with CMS care standards. Based on a national average, CMS penalties for skilled nursing properties had been on the rise from 2016 to the third quarter of 2019.
As the country began to grapple with the COVID-19 pandemic, and the public health emergency was announced, the national average of CMS penalties declined. This was likely a reflection of the more collaborative, less-punitive surveys that took place while surveyors – the CMS regulatory staff who assess compliance with Medicare health and safety regulations – and operators alike learned about COVID-19, it’s spread, and the best practices regarding infection control, PPE stock, and sanitation protocols.
The COVID-19 Public Health Emergency (PHE) was first declared on January 31, 2020 and was most recently renewed for an additional 90 days on October 15, 2021. With no other renewals, this would bring the COVID-19 Public Health Emergency to a duration just a few weeks shy of two entire years.
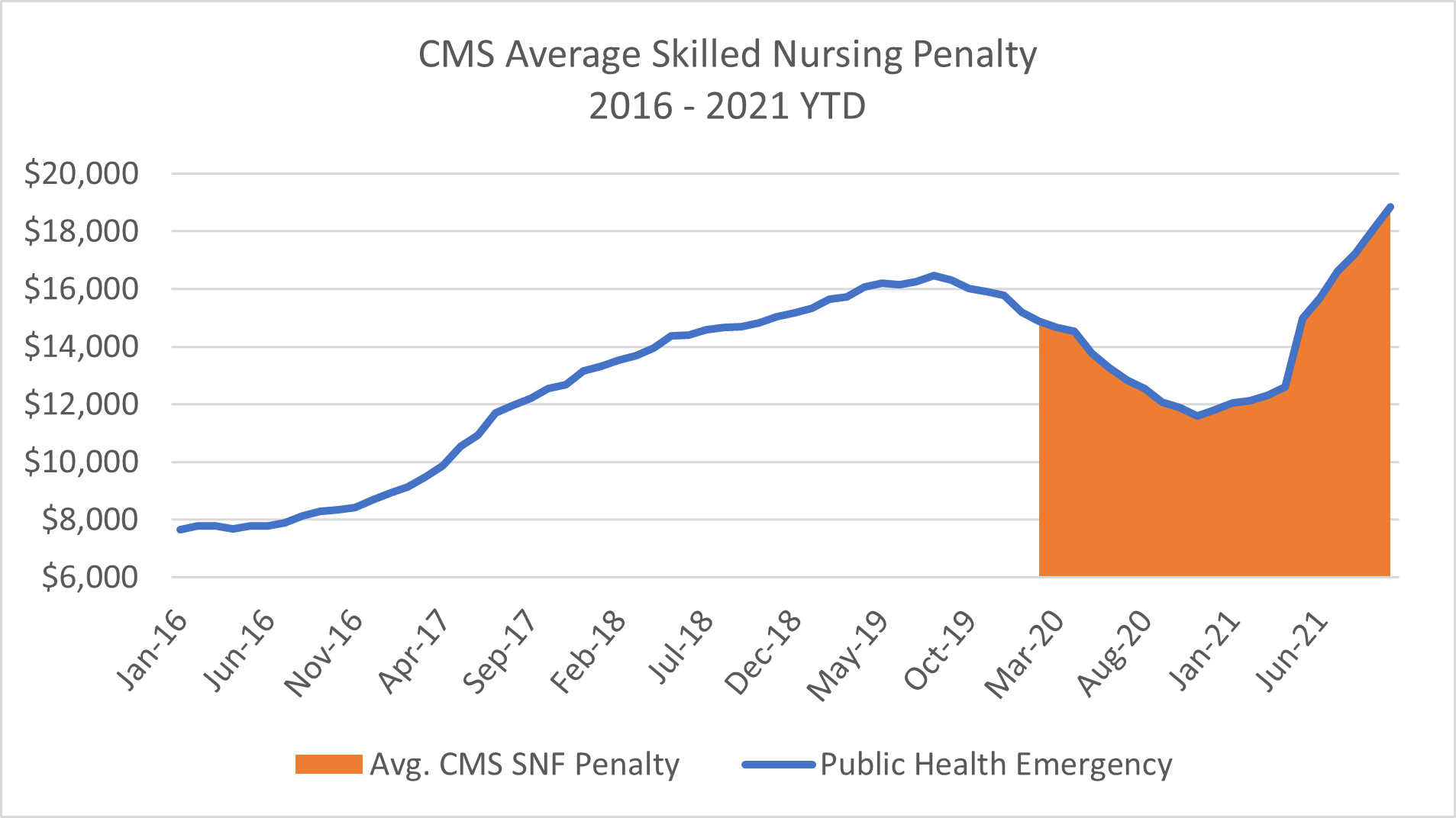
Source: Data.cms.gov; Nursing Home Services Data Archive, 2016-2021
After a downward trend in average CMS skilled nursing penalty during the first ten months of the Public Health Emergency, this metric has now shifted, trending upwards for the past 11 months. The most recently released data from CMS’ Provider Data Set, shows the average skilled nursing penalty at $18,551 for October 2021. This is $2,080, or 12.6%, higher than the pre-Public Health Emergency high mark of $16,471 reported in August 2019.
Two key changes occurred during the COVID-19 Public Health Emergency. First, the understanding about COVID-19 and how to best protect residents grew dramatically. This understanding occurred at many levels – the seniors housing and care sectors, the industry’s regulatory bodies, as well as federal, state, and local governments that all had to get up to speed quickly on best practices regarding the novel coronavirus.
Once that learning curve had been achieved, average CMS skilled nursing penalties began to rise steeply. The rise in average penalty coincided with early vaccination efforts for skilled nursing residents and staff and continued to increase to encourage operators to meet higher staffing ratios, newly identified infection control practices, and sanitation protocols, among other criteria.
In addition to the increasing average CMS skilled nursing penalty, another significant trend has materialized in 2021 – a steep rise in per diem, or per-day, penalties. Skilled nursing properties can be penalized through the imposition of a CMP for either the number of days that a facility has been out of compliance with a federal requirement (per-day or per-diem), for each episode of noncompliance (per-instance), or CMS can deny payments for new admissions.
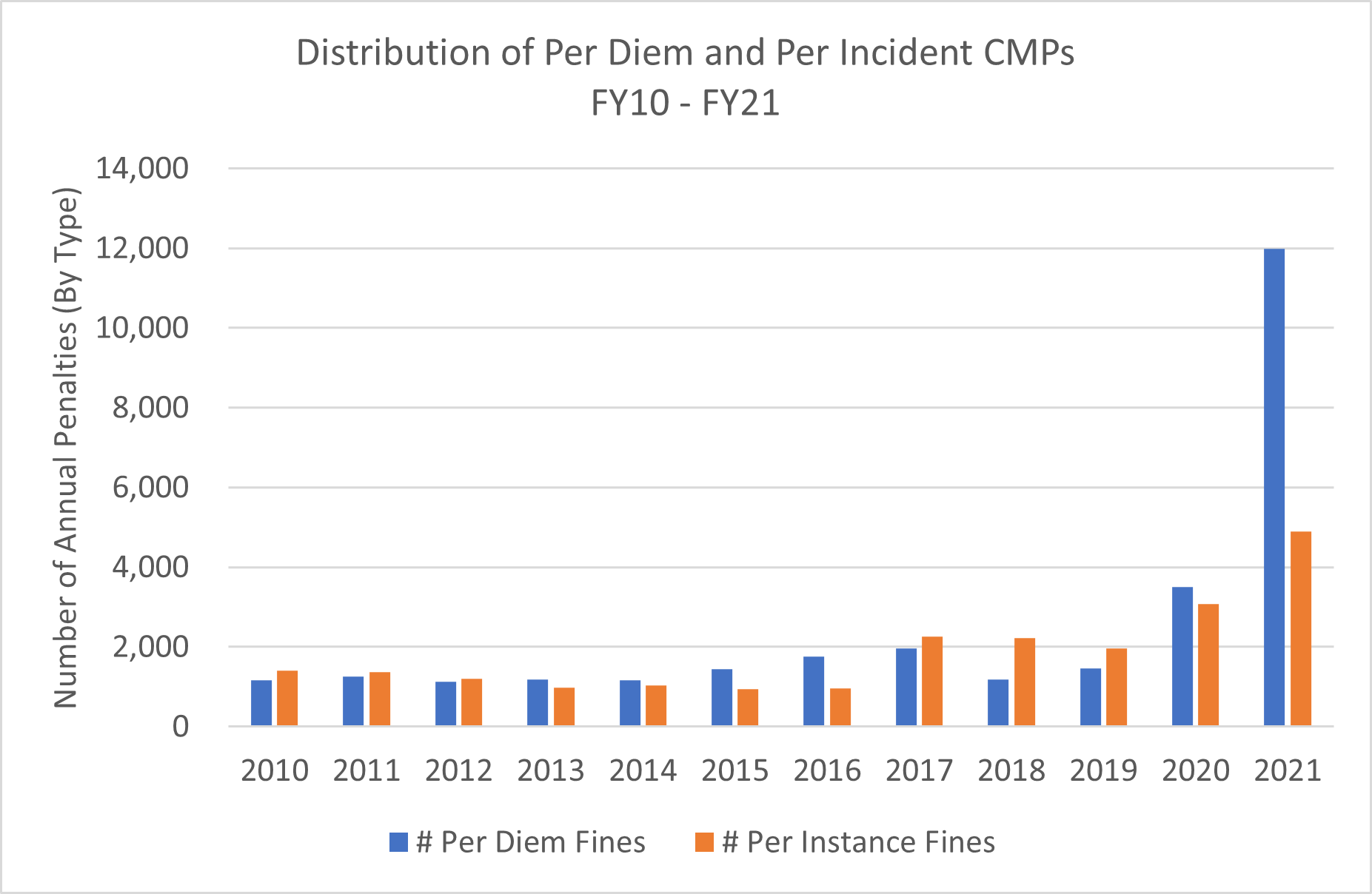
Source: CMS Quality, Certification, & Oversight (QCOR) Reports
In 2017, guidelines were changed to set per-instance CMPs, rather than per-day, as the default penalty. Per-day penalties are often applied retrospectively and can accumulate to significant fines. Although per-day penalties remained the recommended approach for major violations, their overall use has been reasonably limited until 2021.
With a new federal government administration and new leadership at both CMS and HHS, we may be witnessing the return of a stricter survey process. While penalties from CMS are an essential tool for ensuring skilled nursing properties are complying with care standards and are protecting their residents, both the approach to surveying and severity of enforcement may be changing.